- Key Indicators and Measurements: Fetal viability (gestational age, weight, heart rate), placental location (grade, previa), fetal growth (head circumference, abdominal circumference, femur length), amniotic fluid volume (oligohydramnios, polyhydramnios), fetal heart rate monitoring (tachycardia, bradycardia, decelerations), nuchal translucency (Down Syndrome, Edwards Syndrome), structural anomalies (clefts, heart defects, limb abnormalities), blood flow measurements (MCA PSV, umbilical artery PSV), soft markers (echogenic intracardiac focus, nasal bone hypoplasia), anomaly scan (morphology, anatomy), Doppler scan (artery of Adamkiewicz, circle of Willis).
Understanding Red Blue Ultrasound Interpretation
- Explain the key indicators and measurements used in red blue ultrasounds, including fetal viability, placental location, fetal growth, and amniotic fluid volume.
Understanding Red Blue Ultrasound Interpretation
Red blue ultrasounds, also known as Doppler ultrasounds, provide a detailed examination of the fetus during pregnancy. These ultrasounds utilize color-coding to differentiate between blood flow towards and away from the ultrasound transducer, making them invaluable for assessing fetal health and development.
Key Indicators and Measurements
Red blue ultrasounds provide critical information about various aspects of the fetus:
- Fetal Viability: These ultrasounds can assess fetal heart rate, which is a key indicator of the fetus’s health. Additionally, they can determine the fetus’s gestational age, an important measure of fetal growth and maturity.
- Placental Location: Red blue ultrasounds can evaluate the placenta’s location within the uterus. The placenta is responsible for providing oxygen and nutrients to the fetus. Its location can affect fetal growth and the risk of certain complications, such as placenta previa.
- Fetal Growth: These ultrasounds measure various parameters to assess fetal growth, including head circumference, abdominal circumference, and femur length. These measurements help determine if the fetus is growing at a healthy rate.
- Amniotic Fluid Volume: Red blue ultrasounds can measure the amount of amniotic fluid surrounding the fetus. Excessive (polyhydramnios) or insufficient (oligohydramnios) amniotic fluid can indicate potential fetal health issues.
Fetal Viability: Assessing Gestational Age, Weight, and Heart Rate
- Discuss the importance of these measurements in determining the health and development of the fetus.
Fetal Viability: Assessing Gestational Age, Weight, and Heart Rate
During your pregnancy journey, one of the most crucial aspects of monitoring your baby’s well-being is through ultrasound examinations. These scans provide valuable insights into the fetal viability, giving you and your healthcare provider a glimpse into your baby’s health and development.
One of the primary objectives of a red blue ultrasound is to determine fetal viability. This involves assessing the gestational age, weight, and heart rate of your precious bundle of joy. These measurements serve as fundamental indicators of your baby’s growth and vitality.
Gestational Age:
Ultrasound scans accurately estimate the gestational age of your baby, indicating how far along you are in your pregnancy. This crucial information helps monitor your baby’s growth and development throughout each trimester. By comparing the size and maturity of your baby to established norms, your healthcare provider can assess whether your baby is developing on track or if any potential concerns need to be addressed.
Weight:
Determining the fetal weight is another vital aspect of an ultrasound examination. Your baby’s weight provides insights into their overall growth and well-being. By measuring the circumference of your baby’s head and abdomen, the sonographer can estimate their approximate weight. Tracking your baby’s weight throughout your pregnancy helps ensure that they are receiving adequate nutrition and are on a healthy growth trajectory.
Heart Rate:
Monitoring the fetal heart rate is of utmost importance during an ultrasound. Your baby’s heart rate can reveal valuable information about their cardiovascular health and overall well-being. Regular heartbeats indicate a healthy heart function, while abnormal or irregular heartbeats may warrant further investigation. Throughout your pregnancy, your healthcare provider will closely observe your baby’s heart rate to ensure that it remains within a healthy range.
In summary, fetal viability assessments during red blue ultrasounds are essential for monitoring your baby’s gestational age, weight, and heart rate. These measurements provide valuable information about your baby’s development and well-being, allowing you and your healthcare provider to make informed decisions throughout your pregnancy journey.
Placental Location: Evaluating Placental Grade and Placenta Previa
The placenta, a vital organ during pregnancy, plays a fundamental role in the exchange of nutrients and oxygen between the mother and the developing fetus. During regular ultrasound examinations, healthcare professionals scrutinize the location and maturity of the placenta to ensure optimal fetal well-being.
Placental Grade
Placental maturity is assessed by examining its appearance on ultrasound. As pregnancy progresses, the placenta undergoes changes in its structure, termed placental grading. Typically, the placenta is graded on a scale from 0 to 3, with 0 indicating a less mature placenta and 3 representing a fully mature placenta. Understanding placental grade is essential as it can provide insights into the fetus’s overall health and development.
Placenta Previa
Placenta previa is a serious condition that arises when the placenta implants in the lower segment of the uterus, partially or completely covering the cervix. This abnormal placental location can lead to severe complications if left untreated.
Complications Associated with Placenta Previa
Placenta previa can potentially cause:
- Preterm labor: The placenta’s abnormal location can interfere with the cervix’s ability to close during the later stages of pregnancy, leading to premature birth.
- Placental abruption: Placental previa increases the risk of placental abruption, a life-threatening condition where the placenta separates from the uterine wall before delivery.
- Excessive bleeding: During labor, the placenta previa can block the baby’s passage and cause significant bleeding, both for the mother and the baby.
Monitoring and Management of Placenta Previa
To prevent or mitigate complications associated with placenta previa, healthcare providers closely monitor pregnancies with this condition. They:
- Perform regular ultrasounds: Regular ultrasounds track the placenta’s position and assess the risk of complications.
- Order bed rest: This reduces pressure on the placenta and minimizes the risk of bleeding.
- Schedule a cesarean delivery: In most cases, a cesarean delivery is necessary to prevent life-threatening complications during labor.
Fetal Growth: Head Circumference, Abdominal Circumference, and Femur Length
- Describe how these measurements help assess the growth and well-being of the fetus.
Fetal Growth: Measuring for Health and Well-being
Throughout pregnancy, a series of ultrasound examinations are conducted to monitor the growth and development of the fetus. Of paramount importance are three key measurements that provide valuable insights into the well-being of your little one: head circumference, abdominal circumference, and femur length.
Head Circumference
The head circumference is measured around the largest part of the fetal head, providing an indication of its size and overall development. A normal head circumference is crucial for proper brain growth and function.
Abdominal Circumference
The abdominal circumference measures the girth of the fetal abdomen, which is essential for assessing growth, as it correlates with the development of organs and muscles. This measurement also helps identify potential anomalies, such as abdominal hernias or gastrointestinal issues.
Femur Length
The femur, the longest bone in the body, is measured from the top of the hip bone to the knee. This measurement is used to assess fetal size and skeletal development. It is particularly important for detecting growth abnormalities and skeletal disorders.
Assessing Gestational Age and Growth
By comparing these measurements to established norms, ultrasound technicians can accurately determine the gestational age of the fetus. This information helps estimate the expected date of delivery and assess * fetal growth progression*.
Identifying Potential Issues
Deviations from expected measurements may indicate potential growth issues. For instance, a small head circumference or a large abdominal circumference could suggest a growth restriction or a genetic condition. Conversely, an excessive head circumference may raise concerns about hydrocephalus, a condition where fluid accumulates in the fetal brain.
Ensuring Fetal Well-being
Regular monitoring of these growth parameters is crucial for ensuring the well-being of the developing fetus. By pinpointing any deviations early on, healthcare providers can take necessary steps to address potential growth concerns and provide timely interventions if needed.
Amniotic Fluid Volume: Navigating Oligohydramnios and Polyhydramnios
Amniotic fluid, the protective liquid surrounding your baby during pregnancy, plays a crucial role in their development. A healthy balance of amniotic fluid is essential for optimal growth, movement, and organ function. However, imbalances can arise, leading to the conditions of oligohydramnios (insufficient amniotic fluid) and polyhydramnios (excessive amniotic fluid).
Oligohydramnios
When amniotic fluid levels are too low, your baby may experience restricted growth and difficulty with lung development. This condition can also increase the risk of premature birth and limb abnormalities. Oligohydramnios can be caused by various factors, including:
- Uterine abnormalities
- Kidney problems in the baby
- Gestational hypertension
- Amniotic fluid leakage
Polyhydramnios
Excess amniotic fluid can also pose risks to your baby. Premature rupture of membranes (PROM), a condition where the amniotic sac breaks too early, can lead to polyhydramnios. Other causes include:
- Fetal anomalies (such as gastrointestinal defects)
- Multiple pregnancies
- Maternal diabetes
- Infections
Impact on Fetal Health
The amount of amniotic fluid is directly linked to fetal development. Oligohydramnios can restrict the baby’s movement, which can result in physical deformities and complications with the musculoskeletal system. Severely low amniotic fluid levels can even be fatal to the fetus.
Polyhydramnios, on the other hand, can lead to:
- Preterm labor
- Placental abruption
- Fetal malposition
- Cord prolapse
Monitoring and Management
Regular prenatal ultrasounds are crucial for measuring amniotic fluid levels. Early detection of any abnormalities allows your healthcare provider to determine the appropriate course of action. In cases of oligohydramnios, interventions may include increasing fluid intake, administering saline injections, and even amnioinfusion (injecting fluid into the amniotic sac).
For polyhydramnios, management options focus on:
- Monitoring fetal heart rate and movement
- Inducing labor in certain cases
- Amniocentesis (removing excess fluid)
Understanding the importance of amniotic fluid volume is essential for ensuring a healthy pregnancy. By monitoring amniotic fluid levels and promptly addressing any imbalances, you can protect your baby’s well-being and optimize their chances of a successful birth.
Fetal Heart Rate Monitoring: Decoding the Rhythm of Life
During pregnancy, your baby’s well-being is paramount. Monitoring their fetal heart rate is a crucial aspect of prenatal care, providing valuable insights into their cardiovascular health and potential risks.
What is Fetal Heart Rate Monitoring?
Fetal heart rate monitoring involves using ultrasound technology to measure the number of times your baby’s heart beats per minute. This information is recorded over time, creating a graphical representation called a cardiotocograph.
Understanding the Normal Range
A normal fetal heart rate typically ranges from 110 to 160 beats per minute. Rates consistently above this range are considered tachycardia, while rates below the normal range are known as bradycardia.
Tachycardia: A Sign of Distress?
Sustained tachycardia can be an indication of fetal distress. It may occur due to factors such as maternal fever, dehydration, or fetal hypoxia (lack of oxygen). In some cases, it can also be caused by genetic abnormalities or certain medications.
Bradycardia: A Concern for Oxygen Supply
Chronic bradycardia is often associated with reduced fetal oxygen supply. It may indicate conditions such as prematurity, placental insufficiency, or heart defects. Close monitoring is necessary to determine the underlying cause and provide timely interventions.
Decelerations: Clues to Fetal Well-being
Decelerations are temporary decreases in fetal heart rate. They are often classified into various types, each with potential implications:
- __**Early decelerations**_ are typically associated with normal fetal responses to uterine contractions.
- __**Late decelerations**_ may indicate placental insufficiency, likely due to reduced blood flow to the placenta.
- __**Variable decelerations**_ are thought to be caused by umbilical cord compression and are usually not a cause for concern unless they are frequent or prolonged.
Importance of Monitoring
Regular fetal heart rate monitoring is essential for detecting deviations from normal patterns. Early identification of abnormal heart rates allows healthcare providers to take prompt action and address any potential risks to the baby’s health.
By monitoring your baby’s heart rate, you are actively participating in ensuring their well-being throughout pregnancy. It is a simple yet powerful tool that provides peace of mind and allows you to make informed decisions for your little one’s future.
Nuchal Translucency: A Window into Potential Genetic Conditions
During a prenatal ultrasound, one crucial measurement is nuchal translucency (NT). This is the thickness of the fluid-filled space at the back of a baby’s neck. It’s an important indicator used to screen for potential genetic conditions, such as Down syndrome and Edwards syndrome.
Down syndrome is a chromosomal condition caused by an extra copy of chromosome 21. It can lead to a range of developmental delays and health issues. Edwards syndrome is another chromosomal condition, caused by an extra copy of chromosome 18. It’s a more severe condition, often leading to miscarriage or health complications incompatible with life.
Measuring nuchal translucency is a non-invasive procedure that can provide valuable information about the risk of these conditions. Typically, a measurement of 3 millimeters or less is considered normal. A thicker nuchal translucency may indicate an increased risk of Down syndrome or Edwards syndrome.
If the NT measurement is abnormal, further testing may be recommended, such as a chorionic villus sampling (CVS) or amniocentesis. These tests can confirm or rule out a chromosomal condition with greater accuracy.
It’s important to remember that a thickened nuchal translucency is not a diagnosis. It simply indicates the need for further evaluation to assess the risk. A normal nuchal translucency, on the other hand, reduces the chance of these conditions but does not eliminate it completely.
If you have any concerns about your baby’s health, don’t hesitate to discuss them with your healthcare provider. They can provide guidance on the best course of action and help you make informed decisions about your pregnancy.
Structural Anomalies: Uncovering Potential Fetal Concerns
During an ultrasound, detecting structural anomalies is a crucial step in assessing fetal well-being. Identifying clefts, heart defects, and limb abnormalities can provide valuable insight into the health and development of the baby.
Clefts, such as cleft lip and palate, are birth defects that occur when the tissues of the face and mouth do not fuse properly. These anomalies can affect both the baby’s appearance and their ability to feed and speak. Heart defects, ranging from minor holes to complex structural abnormalities, can impact the baby’s cardiovascular system and overall health. Early detection and treatment are essential for managing these conditions.
Limb abnormalities can include missing or shortened limbs, clubfoot, and other orthopedic issues. These anomalies may affect the baby’s mobility and quality of life. By identifying these structural anomalies during pregnancy, healthcare professionals can provide expectant parents with information and support, and plan for potential interventions after birth.
Understanding the significance of structural anomalies is crucial for expectant parents. It allows them to make informed decisions and prepare for the potential challenges and joys that lie ahead with their new bundle of joy.
Blood Flow Measurements: Unraveling the Secrets of Fetal Well-being
The intricate network of blood vessels within your unborn child’s body holds vital secrets about their health and well-being. During prenatal ultrasounds, healthcare professionals meticulously measure the flow of blood through key arteries to assess fetal development and identify potential complications. Two crucial measurements are the MCA PSV (Middle Cerebral Artery Peak Systolic Velocity) and the Umbilical Artery PSV (Peak Systolic Velocity).
The MCA PSV measures the blood flow in the middle cerebral artery, a major artery supplying the brain. Elevated MCA PSV can indicate elevated blood pressure in the fetal brain, which may be a sign of underlying conditions such as fetal anemia or certain genetic syndromes. Conversely, low MCA PSV can suggest insufficient blood flow to the brain, potentially affecting its proper development.
The Umbilical Artery PSV measures blood flow in the umbilical artery, which connects the fetus to the placenta. Increased Umbilical Artery PSV may indicate placental insufficiency, where the placenta is unable to provide adequate oxygen and nutrients to the fetus. This can lead to fetal growth restriction or other complications. Decreased Umbilical Artery PSV may be associated with abnormalities in the fetal heart or circulatory system.
Monitoring these blood flow measurements during prenatal ultrasounds allows healthcare professionals to assess the overall health of the fetus, identify potential problems, and take proactive measures to ensure a safe and healthy pregnancy. By unraveling the secrets hidden within fetal blood flow, these measurements empower healthcare providers to nurture the well-being of the tiny lives they care for.
Soft Markers: Unveiling Potential Fetal Abnormalities
Soft markers are subtle ultrasound findings that may indicate a higher risk of certain fetal abnormalities. While they are not definitive diagnoses, they can serve as clues that warrant further evaluation.
Echogenic Intracardiac Focus (EIF)
An EIF is a bright spot within the fetal heart that may be associated with Down syndrome. It typically appears in the left ventricle of the heart during the first trimester. The presence of an EIF does not necessarily mean Down syndrome, as it can also be seen in normal fetuses. However, it can increase the risk of Down syndrome, especially if combined with other soft markers.
Nasal Bone Hypoplasia (NBH)
NBH refers to an unusually short or absent nasal bone in the fetal face. It is associated with an increased risk of Down syndrome, as well as other chromosomal abnormalities and heart defects. The absence of a nasal bone is more indicative of a problem than a short nasal bone.
Significance of Soft Markers
The presence of soft markers alone does not confirm a fetal abnormality. However, they can alert healthcare providers to the possibility of increased risk and may prompt them to recommend further testing, such as genetic screening or amniocentesis. It’s important to note that soft markers are not always indicative of a problem, and many fetuses with soft markers are born healthy.
Role in Prenatal Care
Soft markers play a valuable role in prenatal care by providing information that can help guide decisions regarding further testing and monitoring. By identifying potential risks early on, healthcare providers can proactively address any concerns and optimize the outcome for both the mother and the baby.
Soft markers are subtle ultrasound findings that can provide insights into potential fetal abnormalities. While they are not diagnostic, they can be useful in assessing risk and making informed decisions about prenatal care. By understanding the significance of soft markers, expectant parents can work closely with their healthcare providers to ensure the best possible pregnancy outcome.
Anomaly Scan: Morphology and Anatomy Scan
- Describe the purpose of these scans in detecting anatomical anomalies and providing a detailed view of the fetal body.
Anomaly Scan: Unveiling the Fetal Body with Clarity
The anomaly scan, also known as the morphology or anatomy scan, is a crucial milestone in prenatal care, providing a comprehensive examination of the developing fetus. This scan takes place between 18 and 22 weeks of gestation and offers an unparalleled opportunity to detect potential anatomical abnormalities and assess the overall well-being of your little one.
Purpose of the Anomaly Scan
The primary objective of the anomaly scan is to identify any developmental concerns or birth defects that may not be apparent through regular prenatal check-ups. By examining the fetal body in detail, doctors can evaluate:
- Brain and skull: To rule out any abnormalities in the brain’s structure or the shape of the skull.
- Face: To check for clefts or any facial deformities.
- Heart: To assess its structure and function, ensuring proper blood flow and heart rate.
- Abdomen: To examine the organs and detect any abnormalities in their position or development.
- Limbs: To verify the presence, length, and alignment of the arms, legs, hands, and feet.
- Spinal cord: To detect any defects or anomalies that may affect the baby’s mobility and development.
Benefits of the Anomaly Scan
Undergoing an anomaly scan provides numerous benefits for both expectant mothers and healthcare professionals. Early detection of potential issues allows for:
- Informed decision-making: Parents can make informed choices regarding the pregnancy and future care based on the scan results.
- Personalized care: Doctors can tailor prenatal care and delivery plans to address any identified concerns.
- Peace of mind: The scan can alleviate parental anxiety by providing reassurance or identifying any necessary interventions.
- Early intervention: If any abnormalities are detected, timely intervention can improve the baby’s chances of a healthy outcome.
The anomaly scan is an essential part of prenatal care, offering a detailed glimpse into the developing fetus and providing valuable information for ensuring a healthy pregnancy. By embracing this scan, expectant mothers and their healthcare providers can work together to promote the well-being of the unborn child.
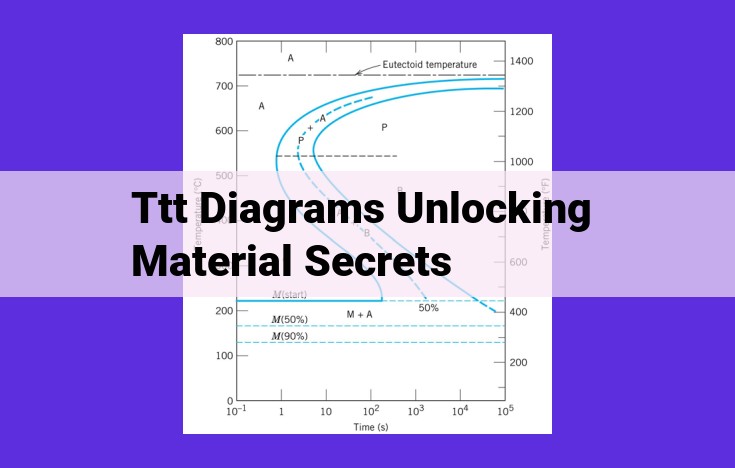
Doppler Scan: Artery of Adamkiewicz and Circle of Willis
During red blue ultrasounds, Doppler scans play a vital role in assessing blood flow to the fetal spinal cord and the brain. These scans provide valuable information about the cardiovascular health of the developing fetus.
Artery of Adamkiewicz
The artery of Adamkiewicz is a major blood vessel that supplies blood to the lower spinal cord. A Doppler scan of this artery can detect abnormalities in blood flow, which may indicate congenital spinal cord defects. By identifying these conditions early, healthcare providers can provide timely intervention to minimize potential neurological damage.
Circle of Willis
Another important Doppler scan is the Circle of Willis. This scan evaluates blood flow within a network of arteries at the base of the fetal brain. Adequate blood flow to the Circle of Willis is crucial for the proper development and functioning of the brain. Doppler scans can detect abnormalities in blood flow that may suggest neurological conditions, such as stroke or heart defects.
Importance of Doppler Scans
Doppler scans are non-invasive procedures that provide essential information about the fetal cardiovascular system. By detecting abnormalities in blood flow, these scans help identify potential health risks and facilitate timely medical intervention. Early detection can significantly improve the prognosis of fetuses with congenital anomalies.
Remember, Doppler scans are an integral part of a comprehensive ultrasound evaluation. Red blue ultrasounds provide a wealth of information about fetal health and well-being, empowering healthcare providers to make informed decisions and ensure the best possible outcomes for both mothers and their unborn children.