This comprehensive guide provides essential knowledge about hypothermia, emphasizing the crucial role of warming IV fluids to prevent complications and safeguard patient well-being. It explores various fluid warming devices and techniques, explaining their advantages and limitations. The guide also clarifies the differences between core temperature, body temperature, and temperature gradient, highlighting their significance in hypothermia management. Furthermore, it offers practical insights into heat conservation and heat production, promoting a deeper understanding of thermoregulation. By implementing the guidelines outlined in this resource, healthcare professionals can effectively manage hypothermia and improve patient outcomes.
Understanding Hypothermia
- Definition and Causes
- Thermoregulation and Heat Exchange
Understanding Hypothermia: The Chilling Reality
Hypothermia, a potentially life-threatening condition, occurs when the body loses heat faster than it can generate it, leading to a dangerously low core temperature. A normal body temperature is around 98.6°F (37°C), while hypothermia sets in when it drops below 95°F (35°C).
Causes of Hypothermia
Hypothermia can strike in various situations, including:
- Exposure to cold: Extreme cold, such as icy water or freezing temperatures without appropriate clothing, can cause rapid heat loss.
- Underlying medical conditions: Certain conditions, like thyroid disorders or diabetes, can impair the body’s ability to regulate temperature.
- Medications and alcohol: Some medications and excessive alcohol consumption can also interfere with thermoregulation.
Thermoregulation and Heat Exchange
Our bodies maintain a constant core temperature through thermoregulation. When the body senses a drop in temperature, it initiates processes to generate heat and conserve it. These processes include:
- Vasoconstriction: Blood vessels in the skin narrow to reduce heat loss.
- Shivering: Involuntary muscle contractions produce heat.
- Metabolic rate increase: The body speeds up its metabolism to generate energy and thus heat.
- Heat production by brown fat: A specialized type of fat tissue that burns fat to produce heat.
- Heat conservation: The body conserves heat by huddling, seeking shelter, or wearing insulating clothing.
The Critical Importance of Warming IV Fluids: Protecting Patients from Hypothermia’s Dangers
In the realm of healthcare, hypothermia poses a significant threat to patients, potentially causing severe complications and even death. With cold IV fluids acting as a major contributor to this condition, warming them is an essential measure for patient safety. This article delves into the importance of warming IV fluids, exploring their role in preventing complications and their impact on core temperature.
When infused unwarmed, cold IV fluids disrupt the body’s thermoregulation system, causing vasoconstriction (narrowing of blood vessels) and shivering. These responses can lead to a cascade of adverse effects, including:
- Cardiac arrhythmias: Cold fluids can trigger abnormal heart rhythms, increasing the risk of cardiac arrest.
- Metabolic disturbances: Shivering and vasoconstriction increase oxygen consumption and energy expenditure, potentially leading to electrolyte imbalances.
- Thrombosis: Cold fluids can promote blood clotting, increasing the risk of deep vein thrombosis (DVT) and pulmonary embolism (PE).
To mitigate these risks, warming IV fluids to body temperature is crucial. Warmed fluids:
- Prevent vasoconstriction and shivering, conserving body heat and reducing stress on the cardiovascular system.
- Improve tissue oxygenation, enhancing metabolic processes and reducing the risk of complications.
- Decrease blood viscosity, minimizing the risk of thrombosis.
Moreover, warming IV fluids has a significant impact on core temperature. When cold fluids are infused, they absorb heat from the patient’s body, lowering core temperature. Conversely, warmed fluids transfer heat to the body, helping to maintain a normal core temperature. This is particularly critical for patients who are already hypothermic or have impaired thermoregulation.
In conclusion, warming IV fluids is an essential measure to prevent complications and maintain core temperature in patients. By understanding the potential risks of cold IV fluids and the benefits of warming them, healthcare professionals can ensure the safety and well-being of their patients.
Fluid Warming Devices and Techniques: Vital in Hypothermia Management
In the depths of a chilly day, as the icy grip of hypothermia threatens, the warmth of an intravenous (IV) fluid can mean the difference between life and death. Understanding how these fluids are warmed and the devices used in the process is crucial for effective hypothermia management.
Fluid Warmers: A Precise Solution
Fluid warmers are standalone devices that heat IV fluids to a precise temperature, ensuring reliable and consistent delivery. They utilize circulating water baths or heating elements to achieve the desired temperature. Their accuracy and efficiency make them ideal for controlled fluid warming, particularly in critical care settings.
Warming Blankets: A Gentle Embrace
Warming blankets envelop the patient in a cozy embrace, transferring heat from the device to the body. They are less invasive than other methods and provide a comfortable way to maintain body temperature. However, their effectiveness may vary depending on the type of blanket and the patient’s condition.
Warming Mattresses: A Comprehensive Approach
Warming mattresses go a step further, providing a heated surface that covers the entire body. They effectively distribute heat, reducing the risk of localized overheating or hypothermia. Their larger surface area also allows for more efficient temperature control.
Forced-Air Warming Systems: Rapid Heat Delivery
Forced-air warming systems utilize a warm air blower to circulate heated air around the patient’s body. **This method offers rapid and effective heat delivery, but it can be noisy and may cause discomfort for some patients.*
Choosing the Right Method: Advantages and Disadvantages
Each method has its own advantages and disadvantages. Fluid warmers provide precise temperature control, while warming blankets offer comfort and less invasiveness. Warming mattresses distribute heat evenly, and forced-air systems provide rapid heat delivery. Selecting the optimal method depends on the patient’s condition, the severity of hypothermia, and the available resources.
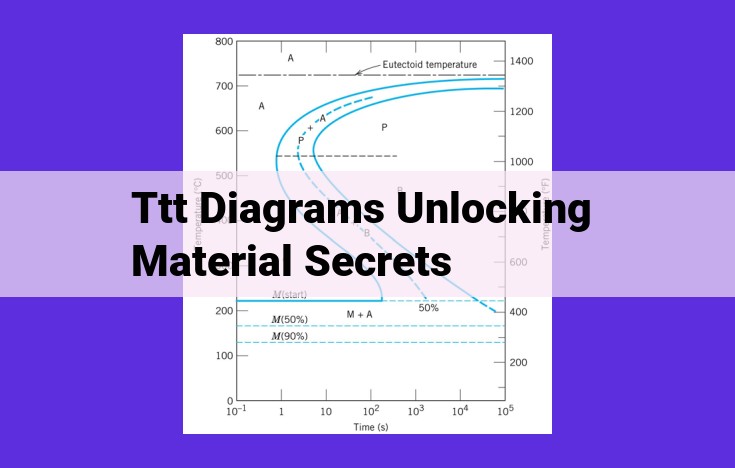
Core Temperature, Body Temperature, and Temperature Gradient: Understanding the Difference and Significance
In the realm of healthcare, understanding the subtle interplay between core temperature, body temperature, and temperature gradient proves critical in effectively managing hypothermia. Each of these concepts holds distinct significance, and their interconnectedness forms the foundation for appropriate treatment strategies.
Differences and Relationships
- Core temperature refers to the temperature of the body’s vital organs, such as the heart, brain, and lungs. It is the most important temperature to monitor and maintain, as it reflects the overall physiological function of the body.
- Body temperature encompasses the temperature of the entire body, including the core and the extremities. While typically lower than core temperature, body temperature still plays a crucial role in regulating overall body heat.
- Temperature gradient refers to the difference between core temperature and body temperature. A significant temperature gradient indicates a problem with thermoregulation, a crucial process that enables the body to maintain a constant internal temperature.
Significance in Hypothermia Management
Hypothermia occurs when the body’s core temperature drops below 95°F (35°C). The lower the core temperature, the more severe the hypothermia. Monitoring core temperature is essential because it provides a direct indication of the body’s thermal status.
In hypothermia, the body’s natural thermoregulatory mechanisms fail, resulting in a decrease in core temperature and a widening of the temperature gradient. The body compensates by constricting blood vessels in the extremities to conserve heat in the core, further exacerbating the temperature gradient.
Understanding the differences and relationships between core temperature, body temperature, and temperature gradient is fundamental for healthcare professionals in effectively managing hypothermia. By monitoring core temperature, assessing the temperature gradient, and implementing appropriate warming strategies, we can ensure the best possible outcomes for patients experiencing hypothermia.
Heat Conservation and Heat Production: Managing Hypothermia
In the battle against hypothermia, understanding how to conserve and produce heat is paramount.
Mechanisms of Heat Conservation
Our bodies employ several mechanisms to retain precious warmth:
- Vasoconstriction: Blood vessels in the skin narrow, reducing blood flow to the extremities and conserving heat in the body’s core.
- Shivering: Uncontrollable muscle contractions generate heat to raise body temperature.
- Goosebumps: Tiny muscles contract, causing hair follicles to stand erect, creating a layer of insulating air.
Processes for Generating Heat
Beyond conserving heat, our bodies also have ways to produce it:
- Metabolism: The body’s chemical processes generate heat as a byproduct. Increased physical activity raises metabolic rate and heat production.
- Thermogenesis: Brown adipose tissue, found in newborns and small mammals, is specially designed to burn fat and produce heat.
Note: While hypothermia poses significant risks to our health, it’s important to remember that our bodies are equipped with remarkable capabilities to maintain homeostasis. By understanding the mechanisms of heat conservation and heat production, we can better support the body’s fight against this condition.
Implementation of IV Fluid Warming: A Crucial Step for Hypothermia Management
Guidelines for Temperature Control
To ensure effective IV fluid warming, adhering to specific temperature guidelines is paramount. Rapid warming methodologies, such as inline fluid warmers, are recommended to raise core temperature rapidly and prevent further heat loss.
However, gradual warming strategies, using insulated blankets or warming mattresses, are preferred in patients with severe hypothermia to avoid re-warming shock. This condition occurs due to the sudden expansion of blood vessels as cold, poorly oxygenated blood returns to the core.
Monitoring and Evaluation of Treatment
Close monitoring of patient response is essential to optimize IV fluid warming. Regular checks of core temperature, body temperature, and temperature gradient help assess the effectiveness of the warming measures.
Core temperature, measured at the rectum, esophagus, or pulmonary artery, is the primary indicator of internal body temperature. Achieving and maintaining a core temperature of 36-37°C (96.8-98.6°F) is the goal of therapy.
Body temperature, measured at the skin surface, reflects the body’s response to warming efforts. Temperature gradient, the difference between core and body temperature, provides insight into the patient’s ability to conserve and regulate heat. A decreasing gradient suggests improved thermoregulation.